MACULAR DEGENERATION
What is Macular Degeneration?
Macular degeneration (MD) is a degenerative retinal eye disease that causes progressive loss of central vision, leaving the side vision intact. Since MD most frequently affects people over the age of 50 and the incidence increases with age, it is commonly referred to Age-related Macular Degeneration or AMD. However, the inherited forms of the disease can also affect young people.
In some cases, AMD advances so slowly that people notice little change in their vision. In others, the disease progresses faster and may lead to a loss of vision in both eyes.
MD affects the macula, the part of the eye that allows people to see fine details such as reading, driving, and recognizing faces.
There are two forms of MD:
Dry MD : This is the more common form and accounts for 90% of all MD
Wet MD : In about 10% of cases, dry MD progresses into wet MD which is the more damaging form and can cause severe vision loss
What causes it?
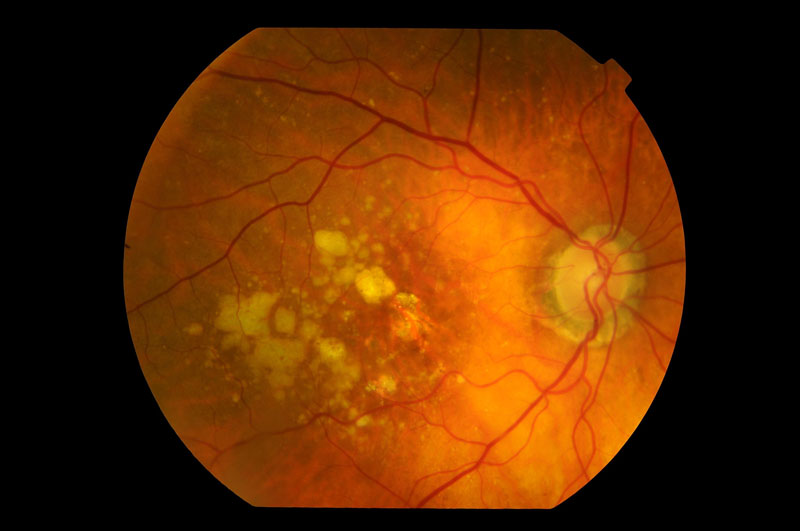
In Dry MD, there is an accumulation of small yellow deposits, known as drusen, under the macula. This phenomena leads to a thinning and drying out of the macula, causing the macula to lose function.
In the Wet form of MD, new blood vessels (choroidal neovascularization) begin to grow underneath the retina and may leak blood and fluid. This leakage causes permanent damage to light-sensitive retinal cells, which die off and create blind spots in central vision.
What are the symptoms?
Patients with Dry MD may have no symptoms with good central eyesight, or a range of vision problems with substantial functional limitations, including:
Blurred vision
Fluctuating vision
Distorted or crooked vision
Difficulty reading, watching TV, driving or recognising peoples’ faces
Limited vision at night or under conditions of reduced illumination.
Progression of symptoms in Dry MD usually occurs slowly
Symptoms of Wet MD may be similar to those of Dry MD however often occur more quickly (over weeks rather than months) and include:
Distorted vision where straight lines appear wavy or bent
Blurred vision
Central scotomas (shadows or missing areas of vision)
Trouble discerning colours; specifically dark ones from dark ones and light ones from light ones
Difficulty reading, watching TV, driving and recognising peoples’ faces
Who is at risk?
The risk for developing macular degeneration increases with age. Other risk factors include:
Family history of macular degeneration
Smoking
Obesity
A high fat diet, and/or one that is low in nutrients and antioxidants
High blood pressure and cardiovascular disease
Prolonged sun exposure
How is it diagnosed?
A comprehensive eye examination will be performed and may include tests such as Retinal photography, Optical Coherence Tomography (OCT), Fluorescein Angiography (FFA) and Indocyanine Green Angiography (ICG) to allow observation of retinal changes, swelling and/or leakage.
Can it be treated?
Currently, there is no treatment available to reverse established damage from dry macular degeneration. However there are ways to slow down the progression and prevent deterioration to more advanced types of macular degeneration. Dry macular degeneration can develop into the more rapidly progressive wet type of macular degeneration, particularly if there are larger amounts of drusen.
Hence, it is important to maintain a healthy lifestyle that may help to prevent or slow progression of dry MD. It Includes:
Taking nutritional supplements which include Vitamins C,E, Zinc and Lutein
Quit Smoking
Wearing sunglasses with UV (ultraviolet light) protection
Keeping blood pressure and cholesterol levels within normal ranges
Having a diet rich in leafy green vegetables and fish
For the Wet type of MD, at present, there are a number of possible treatment options that target the abnormal blood vessels. These treatments do not ‘cure’ the nature of the disease; rather they may help to reduce further vision loss, slow its progression, and improve vision.
Intravitreal injections of Anti-VEGF medications (into the eye)
Photodynamic Therapy (“Cold Laser”)
Thermal Laser Photocoagulation (“Hot Laser”)
Intraocular steroid injections
Our Retina Specialists will determine which treatment will be the most effective for each patient’s eye condition.
Importantly, if there is macular degeneration in one eye, then the fellow eye is at a high risk of developing macular degeneration as well. Hence, early detection and treatment are crucial which means regular check-ups and reporting any noticeable change in vision. If wet MD is treated early, often there is less damage and patients may have better vision with less chance of blindness.